Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
Equal Access to Home Dialysis
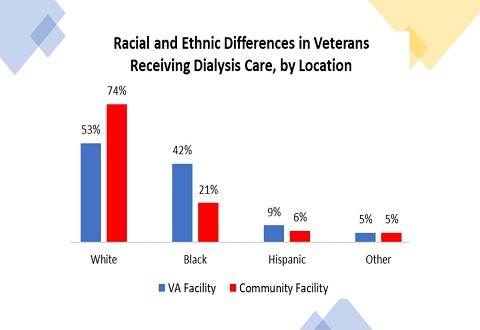
Compared to Veterans who receive dialysis in the community, Veterans who receive dialysis within the Veterans Health Administration (VHA) are more likely to be Black or Hispanic, service connected, have a lower income, and live further from their dialysis provider. They are also more likely to have post-traumatic stress disorder or a history of homelessness. VHA champions the elimination of health disparities for all Veterans, and Dr. Yuvaram Reddy’s research focuses on expanding the availability of home dialysis for Veterans with kidney failure.
By Carson Connor Clark
Friday, March 25, 2022
Yuvaram Reddy, MBBS, MPH, a physician-scientist dedicated to improving home dialysis use for patients with kidney failure, joined CHERP’s Philadelphia site in July 2021. He is a staff Nephrologist at the Michael Crescenz Medical Center and a health equity researcher focused on understanding the barriers to home dialysis use for Veterans and developing new ways to improve and expand home dialysis for vulnerable populations. Dr. Reddy’s work is featured in an informational brief issued by the VA Office of Health Equity on Chronic Kidney Disease and Dialysis in Veterans on March 25, 2022.
We interviewed Dr. Reddy about his VA Research aims, and his commitment to health equity for all Veterans.
Q. What inspired you to focus on home dialysis?
A. I discovered home dialysis early on in my medical training at Boston Medical Center when I cared for patients with kidney failure who performed home dialysis and seemed more in control of their health. I was surprised to learn that, for most patients, home dialysis improves quality of life at lower costs than in-center hemodialysis. However, despite the many benefits, very few patients perform home dialysis, and there are wide disparities in access to this therapy. Puzzled by the underuse of home dialysis, I decided to dedicate my research career to developing tools to improve access to home dialysis for people with kidney failure.
Q. How would you summarize your short- and long-term research goals?
A. Right now, I am studying barriers to home dialysis use so that I can develop strategies to improve access to home dialysis. Specifically, we are asking patients, providers, and healthcare leaders across the country for their perspective on why home dialysis is underused, and how we can improve home dialysis use. With these insights, we plan to develop, test, and implement strategies to make it possible for all patients with kidney failure to have fair and equitable access to home dialysis.
Q. Why is your area of research important to Veterans and the VA?
A. Frankly, kidneys are underappreciated, and kidney disease is very common among our Veterans. Our kidneys are complex organs that protect several organs, including the heart, blood vessels, bones, and red blood cells. Unfortunately, nearly one in six Veterans within the VA have some amount of chronic kidney disease, and many are unaware of their kidney disease.
Each year, nearly 13,000 Veterans develop kidney failure—the last stage of chronic kidney disease—and fewer than 5% of these Veterans receive home dialysis. Instead, most Veterans with kidney failure travel 3 times per week to a dialysis unit for in-center hemodialysis – a therapy that tends to be rigid and demanding. If we can make home dialysis easier to access, and easier to perform, we could help Veterans maintain their independence and quality of life at home.
Q. What drew you to becoming a VA physician and researcher?
A. I’ve been fortunate to serve our Veterans as a physician and researcher during residency, fellowship, and now as faculty at CHERP. VA provides an excellent learning environment in the largest integrated health system in the US! VA also has extraordinary implementation scientists, leaders, and operational partners. The VA is at the cutting edge of implementing research results into patient care, making it a great place to efficiently develop, test, and implement strategies to improve healthcare delivery. Overall, the VA is unparalleled in its dedication to providing high quality care and to implementation science.
Q. What are some examples of research you have done/findings you have published in this area that you anticipate applying to your future VA work?
A. My research and quality improvement projects have two broad themes: 1) evaluating home dialysis barriers to develop novel home dialysis strategies, and 2) evaluating the impact of health policies on health equity.
1. Home dialysis barriers: We are currently analyzing our national survey on barriers to home dialysis use, and I anticipate sharing findings with the community soon. Findings from the survey, along with input from CHERP’s Veterans Community Advisory Board, inform our on-going applications for research funding to evaluate variations in home dialysis use across the VA healthsystem. This will be an exciting opportunity to leverage community and stakeholder input to evaluate home dialysis use within the VA.
2. Health policy: As a result of a new federal executive order for kidney disease, the Centers for Medicare and Medicaid Services (CMS) implemented new payment models in 2021 to promote home dialysis and kidney transplantation. Concerned about the unintended consequences of these payment models on vulnerable patient populations, we published an article discussing strategies to improve health equity in these models. Following our publication, CMS revised the model to include a health equity incentive for providers—making this the first model in CMS’ history to directly incentivize health equity. Now that the model is well underway, we secured funding from the Leonard Davis Institute to understand whether this health equity incentive improves home dialysis and kidney transplantation for all patients with kidney failure.
Q. What advice do you have for others who are interested in a VA research career?
A. There are many VA scientists who are eager to help trainees find their footing. The VA has also created several training opportunities such as post-doctoral fellowships, diversity supplements for VA Merit and QUERI projects, and the National Clinical Scholars Program. Please reach out if you’re interested. The VA is an excellent environment for research training and collaboration.



















